Do you or a loved one have glaucoma? It’s a prevalent age-related eye condition. In fact, it’s one of the leading causes of blindness in adults over the age of 60.
Like many age-related conditions, it often doesn’t show symptoms until the later stages of the disease. Because of the lack of discernible symptoms, glaucoma is often hard to notice until it’s already caused significant visual loss.
Luckily, your ophthalmologist can diagnose it during the early stages simply by having regular eye exams. While there is no cure for glaucoma, you can effectively treat and manage the condition with medication, surgery, or a combination of both. Keep reading to learn more about glaucoma!
Causes
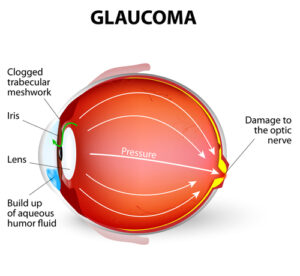
Glaucoma is the name for a collection of diseases that cause damage to the optic nerve. The optic nerve is a vital part of the eye that takes light signals that pass through your vision and translates them into images your brain can understand.
When the optic nerve suffers any damage, it can cause significant gaps in a person’s vision. While glaucoma’s exact causes are still unknown, it is associated with advanced age and high intraocular pressure, or IOP.
Increased intraocular pressure occurs when there’s a buildup of fluid in the eye. There are also several kinds of glaucoma. The two most common are open-angle glaucoma and angle-closure glaucoma. The “angle” referred to in both names is the drainage angle between the cornea and iris.
When the angle becomes blocked, this is angle-closure glaucoma. Pressure builds quickly when the iris bulges and closes the gap between itself and the cornea, preventing any fluid from flowing out through the angle.
The pressure is what causes damage to the optic nerve. This kind of glaucoma is less common but can occur suddenly and requires immediate attention.
By far, the most common form of glaucoma, though, is open-angle glaucoma. The channel between the cornea and iris is open, but the semi-permeable tissue surrounding the angle, called the trabecular meshwork, becomes clogged.
Pressure builds in the eye over time, causing gradual damage to the optic nerve. It is this gradual damage to the optic nerve that results in vision loss.
Risk Factors and Symptoms

The patients at high risk for glaucoma meet one or more of the following criteria:
- Being over 60
- Having high blood pressure, heart disease, or diabetes
- Being of African-American, Latino, or Asian descent
- Having a high refractive error, either nearsightedness or farsightedness
- Prolonged use of corticosteroids
- Experiencing a traumatic eye injury
- Having a family history of glaucoma
Anyone at high risk should see an eye doctor regularly. The earlier you can receive a diagnosis of glaucoma, the better.
An earlier diagnosis increases the chances of being able to save your remaining vision. Open-angle glaucoma especially has very few symptoms until irreversible damage has already occurred. These symptoms include blind spots and eventual tunnel vision in the very late stages.
Acute angle-closure glaucoma causes more severe symptoms, including headache, nausea, general eye pain, bright halos, and eye inflammation. If you experience these symptoms, seek medical help immediately, as angle-closure can cause massive visual loss in a short amount of time.
With glaucoma, any damage is irreversible, meaning that once vision loss has occurred, you cannot restore it. This is why having regularly scheduled eye exams with your eye doctor are so important.
Treatment

There are many different treatment options for patients with glaucoma. The first is medication. Most eye doctors will begin with eye drops that aim to reduce your IOP.
If these don’t work, your eye doctor may supplement medication with surgical techniques. The most common glaucoma surgery is called a trabeculectomy.
A trabeculectomy is a procedure where a small opening is made through the front of the eye to help drain fluid from the eye, helping to lower intraocular pressure. Many other procedures that treat glaucoma are variations of the trabeculectomy.
Laser trabeculoplasty and iridotomies use a laser to create an opening in the trabecular meshwork and through the iris. Other procedures focus on lowering fluid production, like endocyclophotocoagulation (ECP) and transscleral cyclophotocoagulation (CPC). Both of these procedures use laser technology to target fluid-producing tissue and cells.
MIGS Glaucoma Surgery
If you want glaucoma procedures that are less invasive and have less recovery time than traditional glaucoma surgeries, MIGS may be the answer. MIGS stands for Micro Incisional Glaucoma Surgery.
iStent
These procedures are ideal for patients who have yet to experience vision loss from glaucoma. One of the most popular MIGS is the iStent.
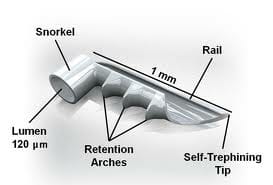
The iStent is the world’s tiniest medical device that’s currently available! This small device gets implanted in the eye and drains fluid to lower IOP.
The beauty of the iStent is you have it implanted during your cataract surgery, allowing you to achieve clear vision and lower intraocular pressure at the same time.
Hydrus microstent
Other MIGS procedures use stents, like the Hydrus microstent. Both devices are so small that patients can’t even feel them after having them implanted.
Dr. Wolff and Westafer have experience performing nearly all common MIGS procedures, including GATT, the OMNI, Kahook Dual-Blade, and ABiC.
There are so many options when it comes to glaucoma treatment that it may seem overwhelming. The treatment that works best for one patient may not work for another.
It’s important to follow your eye doctor’s recommendation regarding treatment and consider all the options available. Keep in mind that MIGS works best for patients with early-stage or moderate glaucoma.
Traditional glaucoma surgeries and laser surgeries are still the best options for anyone with severe glaucoma.
If you’re unsure if you have glaucoma, the first step is to schedule an appointment with your eye doctor. Early diagnosis and treatment are always the best solutions for any eye condition, including glaucoma.
Do you need to see an eye doctor to determine if you may have an eye condition like glaucoma? Schedule an appointment at Sierra Nevada Eye Center in Reno, NV, today!


